Blood Group Test
1. Understanding Blood Groups: The ABO and Rh Systems Blood groups are determined by specific antigens present on the surface of red blood cells. The two most important blood group systems are the ABO system and the Rh system:
ABO System: This system classifies blood into four main groups: A, B, AB, and O. These groups are determined by the presence or absence of antigens A and B on the red blood cells’ surface. Additionally, individuals with blood group AB are universal recipients, while those with blood group O are universal donors.
Rh System: The Rh system, also known as the Rh factor or D antigen, determines whether a person’s blood is Rh-positive (presence of the D antigen) or Rh-negative (absence of the D antigen). This classification is crucial during pregnancy and transfusions, as Rh incompatibility can lead to severe complications.
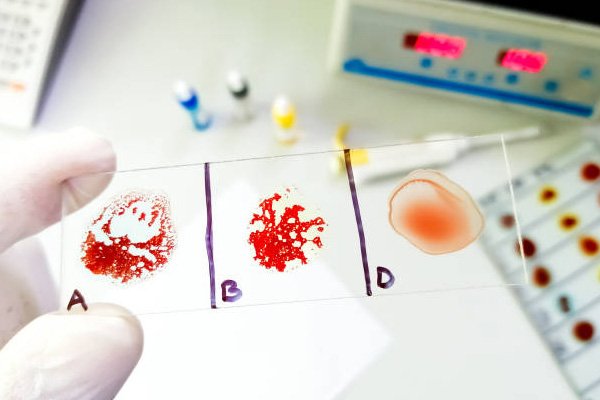
2. The Blood Group Test: Simple and Essential The Blood Group Test is a routine procedure performed in central diagnostics laboratories. It involves a small blood sample collected from the patient’s vein. The blood is then tested for the presence or absence of ABO and Rh antigens using specific antibodies. The result provides information about the individual’s blood group, enabling medical professionals to make informed decisions regarding blood transfusions and medical treatments.
3. Importance in Transfusion Medicine Blood group testing is of utmost importance in transfusion medicine, where it ensures safe and compatible blood transfusions. Matching the recipient’s blood group with the donor’s blood group is crucial to prevent adverse reactions that could be life-threatening. For example, if a person with blood group A receives blood from a donor with blood group B, it could trigger an immune response leading to serious complications.
4. Significance in Prenatal Care In prenatal care, blood group testing is essential to identify any potential Rh incompatibility between the mother and the fetus. Rh incompatibility can occur if the mother is Rh-negative, and the baby is Rh-positive. In such cases, special medical interventions may be required to prevent hemolytic disease of the newborn (HDN), a condition that can result in severe anemia and jaundice in the baby.
5. Organ Transplantation Blood group testing is a critical step in organ transplantation to ensure compatibility between the donor and the recipient. A mismatch in blood groups can trigger an immune response and lead to organ rejection, jeopardizing the success of the transplant.
6. Emergency Situations In emergency situations, when rapid blood transfusions are necessary, knowing the patient’s blood group becomes even more crucial. Immediate access to blood group information can save precious time and potentially life-saving decisions.
7. Future Developments While the fundamental principles of blood group testing remain unchanged, technological advancements and automation in central diagnostics laboratories are streamlining the process, leading to faster and more accurate results. Additionally, ongoing research may unveil more refined subtypes and nuances within the ABO and Rh systems, further enhancing the understanding of blood compatibility.
